Background:
Late-onset hemorrhagic cystitis (LO-HC) is one of the common complications and major causes of morbidity in patients undergoing allogeneic hematopoietic stem cell transplantation (allo-HSCT). The classic treatment for HC includes hydration, alkalization, bladder irrigation, immunosuppressant reduction, and platelet transfusion. When the HC was considered to be associated with aGVHD, more immunosuppressive agents such as glucocorticoids will be added in. However, too intensive immunosuppressive measures leave the patients susceptible to infection and, in turn, increases the accidence of non-relapse mortality (NRM). It is important to explore novel, less-toxic, more effective, and cost-effective strategies for LO-HC. Hyperbaric oxygen therapy (HBOT) can stimulate fibroblast proliferation, angiogenesis, and wound healing. We deduce that HBOT might benefit patients with LO-HC after allo-HSCT.
Methods:
In this study, we retrospectively analyzed 238 patient underwent allo-HSCT in our center. From 2018, patients with LO-HC have been given HBOT in addition to conventional treatment in our center. The data in HBOT and the control group were collected and compared. Patients' characteristics were compared using the x2 test in case of discrete variables or the Mann-Whitney test in case of continuous variables. Logistic regression examined factors might be used as effective predictors for HBOT. Sensitivity and specificity were estimated based on four parameters cut-off point for additional glucocorticoid necessity.
Results:
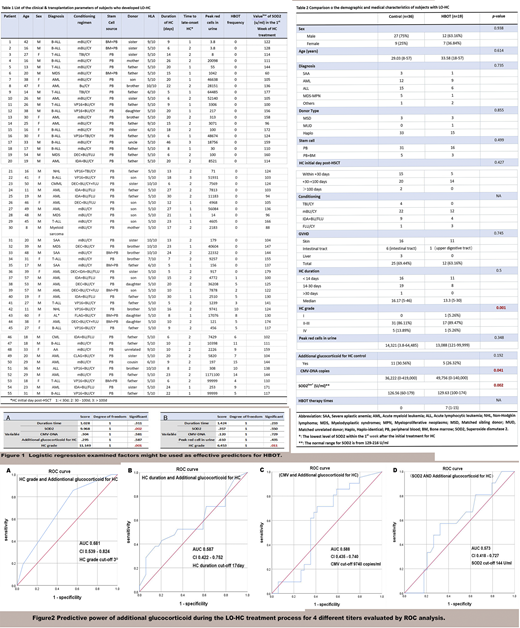
A total of 238 patients who underwent allo-HSCT from 2014 to 2020 were enrolled in this study. Among them, 55 (23.11%) developed LO-HC (36 received regular treatment, and 19 received HBOT in addition to the regular therapy). The clinical & transplantation parameters of the patients with LO-HC were listed in table 1.
There is no significant difference in the age, gender, primary disease distribution, conditioning regimen, donor, HLA compatibility, stem cell sources, the occurrence of aGVHD between two groups. There is also no significant difference in the initial day of LO-HC post-HSCT and duration, peak red cells count in the urine, and whether additional glucocorticoid for HC control had been added between the two groups. It is worth noting that compared with the HBOT group, we found higher HC grade distribution, higher CMV-DNA copies, and decreased levels of SOD2 within the 1st week of the initial therapy for LO-HC in the control group. The comparison of the demographic and medical characteristics of subjects with LO-HC were listed in table 2.
According to the results of logistic regression analysis, patients who developed LO-HC with higher HC grade (p = 0.001) and decreased SOD2 level (p = 0.002) might benefit more from HBOT, indicating that they might be used as effective predictors for HBOT (Figure 1A). Only higher HC grade (p = 0.011) could predict whether or not additional glucocorticoid would be necessary for LO-HC control (Figure 1B).
The predictive power of additional glucocorticoid during the LO-HC treatment process for 4 different titers (HC grade and duration, CMV, and SOD2 level) was evaluated by ROC analysis. According to the area under the curve (AUC), the best diagnostic capabilities of four parameters were shown in Figure 2A, 2B, 2C, and 2D.
None of our patients experienced severe adverse events of HBOT, such as gas emboli, pulmonary edema, and seizures. Only one patient with AML discontinued after 1 session due to the reversible ear barotrauma which was suspected with HOBT.
Conclusions:
In summary, HBOT was effective and well-tolerated in patients with LO-HC post-allo-HSCT. Patients who received HBOT exhibited with short disease duration and mild LO-HC grade. Higher HC grade and decreased SOD2 levels might be used as effective predictors for HBOT. Higher HC grade might be used as a predictor to determine whether or not additional glucocorticoid would be necessary for HC control. In the future, HBOT might be not only used as an adjunctive care application for LO-HC, but also might be as the first-line treatment therapy for this population, regardless of the causes of LO-HC. Based on our preliminary result, we plan to enroll more eligible patients to establish the definitive efficacy and safety of HBOT in patients with LO-HC after allo-HSCT (NCT04502628).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal